Introduction: Among patients with MDS, it is estimated that 17-82% (median 60%) are transfusion dependent (Harnan S, et al. Acta Haematol 2016;136:23-42) and require ≥ 1 unit of red blood cells (RBCs) every 8 weeks. Sufficient blood supply is essential for the administration of RBC transfusions in patients with MDS, as shortage of blood supply may create unnecessary burden, such as treatment delay, worsened quality of life, or increased healthcare utilization. To our knowledge, no studies have examined the physicians' experience associated with shortage of blood supply and RBC transfusion delays in this patient population. Physicians' perspectives on the factors that impact clinical, economic, and humanistic outcomes of patients with MDS are also not well understood. The current study investigated physicians' understanding of these topics.
Methods: Prior to data collection, interviews were conducted with physicians (3 each in France, Germany, Italy, Spain, and the UK) to pre-test and revise the questionnaire, a 40-minute web-based physician survey via the M3 Global Research physician panel, for relevance and understanding. All physicians took the survey in their native language and had to have been in practice for 2-35 years, spend ≥ 75% of their time in direct patient care, and have managed ≥ 15 patients with MDS in the past 3 months. Physicians answered questions regarding adequacy of blood supply related specifically to RBC transfusions for patients with MDS. Physicians identified the top 10 factors (from a list of 32) impacting the clinical, economic, and humanistic outcomes of patients with MDS. These factors were then weighted accordingly (assigned point values summing up to 100). Results were described descriptively in proportions for categorical/ordinal data and mean (standard error [SE])/95% confidence intervals [CI]) for continuous data.
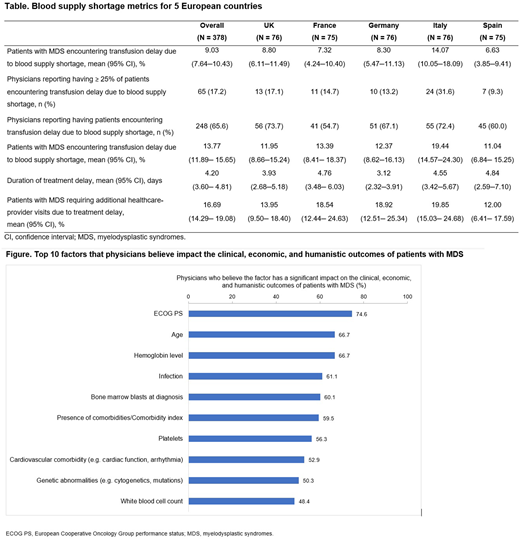
Results: A total of 244 hematologist/oncologists, 124 hematologists, and 10 oncologists completed the survey in France, Germany, Italy, Spain, and the UK (n = 75 [approx.] in each country; Table). On average, physicians were in clinical practice for 14.70 years (SE 0.32), 41.3% were aged 45-54 years, and 64.3% were male. Physicians spent 88.7% (SE 0.36%) of their professional time in patient care, and had seen an average of 54.5 (SE 2.26) patients with MDS in the past 3 months. Over 65% of physicians (range 54.7 [France]-73.7% [UK]) reported that their patients with MDS encountered RBC transfusion delays due to blood supply shortage (Table). On average this impacted 9.0% (95% CI 7.6-10.4) of all patients with MDS. However, among physicians who reported delays (n = 248), 13.8% (95% CI 11.9-15.7) of patients were impacted, ranging from 11.0% (Spain) to 19.4% (Italy). Physicians (17.2%; range 9.3 [Spain]-31.6% [Italy]) reported ≥ 25% of their patients with MDS requiring transfusions experienced transfusion delay due to blood supply shortage. On average, patients experienced a 4.2-day (95% CI 3.6-4.8) delay in receiving a transfusion due to blood supply shortage, and 16.7% (95% CI 14.3-19.1) of patients required additional healthcare provider visits due to blood supply shortages. The top 10 factors reported that impact clinical, economic, and humanistic outcomes of patients with MDS included: Eastern Cooperative Oncology Group performance status (ECOG PS) (74.6%); age (66.7%); hemoglobin level (66.7%); infections (61.1%); percentage bone marrow blasts at diagnosis (60.1%); comorbidities (59.5%); platelets (56.3%); cardiovascular comorbidity (52.9%); genetic abnormalities (50.3%); and white blood cell count (48.4%). Factors that had the greatest mean impact scores were ECOG PS (8.9, 95% CI 8.1-9.8); percentage bone marrow blasts at diagnosis (8.3, 95% CI 7.3-9.2); age (7.2, 95% CI 6.5-8.0); hemoglobin level (6.8, 95% CI 6.1-7.4); and comorbidities (6.6, 95% CI 5.9-7.3).
Conclusions: Two thirds of physicians reported that shortage of blood supply resulted in a delay in RBC transfusions for patients with MDS. Almost 20% reported ≥ 25% of their patients with MDS requiring transfusions experienced a transfusion delay due to blood supply issues. ECOG PS, hemoglobin level, and age were the top factors reported to impact outcomes of patients with MDS. New treatment options should be explored to help reduce the number of RBC transfusions, which may also help improve clinical, economic, and humanistic outcomes of patients with MDS.
Gupta:Bristol Myers Squibb: Consultancy, Research Funding; Kantar: Current Employment. Kulasekararaj:Alexion Pharmaceuticals Inc.: Honoraria, Membership on an entity's Board of Directors or advisory committees. Constantino:Kantar: Current Employment. Grisolano:Kantar: Current Employment; Bristol Myers Squibb: Consultancy. Tang:Bristol Myers Squibb: Current Employment; Asclepius Analytics: Current Employment. Jones:Bristol Myers Squibb: Current Employment. Tang:BMS: Current Employment, Current equity holder in publicly-traded company.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal